The problem of excessive bleeding has been known for millennia, and is mentioned in the Jewish Talmud and the New Testament. In 1803, John Conrad Otto, a Philadelphia physician, first described a hereditary bleeding disorder affecting males; he called them “bleeders.” The term “haemorrhaphilia” — which eventually became “hemophilia” — was first used in 1828 by Friedrich Hopff, a Swedish medical student. It was not until 1947 that “hemophilia” was found to be two separate diseases, hemophilia A and hemophilia B.
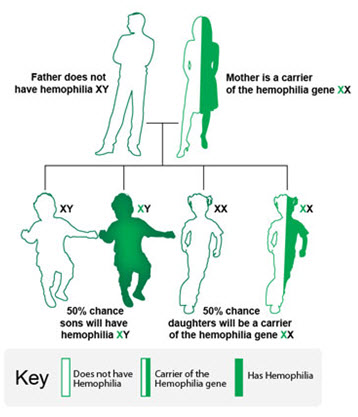
The Royal Disease: Although it is a relatively rare disorder, hemophilia played a significant role in the history of Europe, and became known as “the royal disease.” England’s Queen Victoria passed the gene for hemophilia B to her son Leopold, and two daughters, Alice and Beatrice. The disease eventually spread through the royal houses of Spain, Germany, and most famously to Alexei, the son of Nicholas II, the last Tsar of Russia.
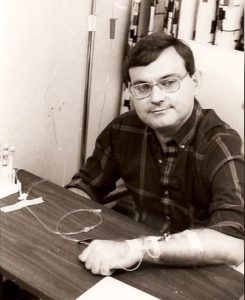
Early Treatment: Before the early 1960s the only treatment for bleeding was a transfusion of whole blood or plasma, usually in a hospital. The average life expectancy of a person with severe hemophilia was 20 years. In 1965 came the discovery of cryoprecipitate—a product rich in clotting factor—that formed when frozen plasma was thawed. By the 1970s, freeze-dried powdered factor concentrates became available. This revolutionized hemophilia care, making it possible for patients to “self-infuse” factor products at home.
The AIDS Crisis: In the late 1970s hemophilia was again in international news as the blood supply became contaminated with hepatitis C and HIV, the virus that causes AIDS. This contamination carried over into the factor concentrates that were just coming into wide use. Thousands of hemophiliacs around the world were infected, including an estimated 10,000 in the United States. In many cases loved ones also unknowingly became infected; thousands died.

On to the Present Day: Thanks to the advocacy of the bleeding disorders community, there are much higher standards for blood collection and the production of factor concentrates. Plasma-derived products are safe. The use of recombinant DNA technology advanced, and new synthetic products that do not use blood, and cannot transmit viruses, have become the standard treatment.
Learn more about this important history from the Hemophilia Federation of America and the National Hemophilia Foundation.